
58-Year-Old African American Female with Diabetes and Uncontrolled Hypertension
February 14, 2024Personalized Treatment Regimen Following Pulse Wave Analysis
70-Year-Old Female with Chronic Kidney Disease and Hypertension
Patient Medical History
- 70-year-old female with chronic kidney disease stage 4 (estimated glomerular filtration rate 28 mL/min/1.73 m2)
- Current Rx Regimen
- Chlorthalidone 25 mg daily
- Carvedilol CR 20 mg daily
- Lisinopril 20 mg daily
Initial Digital Vascular Biomarker Assessment
| Brachial Blood Pressure | 177/56 mmHg |
| Central Systolic Pressure | 171 mmHg |
| Central Pulse Pressure | 115 mmHg |
| Augmentation Index | 44% |
| Heart Rate | 46 bpm |
Initial Assessment Interpretation
This female patient’s central pressure profile indicates a pulse pressure amplification of 5%. The central systolic pressure of 171 mmHg is higher than the desired value of < 124 mmHg. The Augmentation Index (AIx) is about 44%. In this patient scenario, the onset of the second peak is found in the aortic pressure contour at approximately 120 mmHg. With a central pulse pressure of 115 mmHg, this indicates that about 51 mmHg of the 115 mmHg, ie, an AIx of approximately 44%, central pulse pressure is augmented pressure.
Figure 15. Central Pressure Waveform
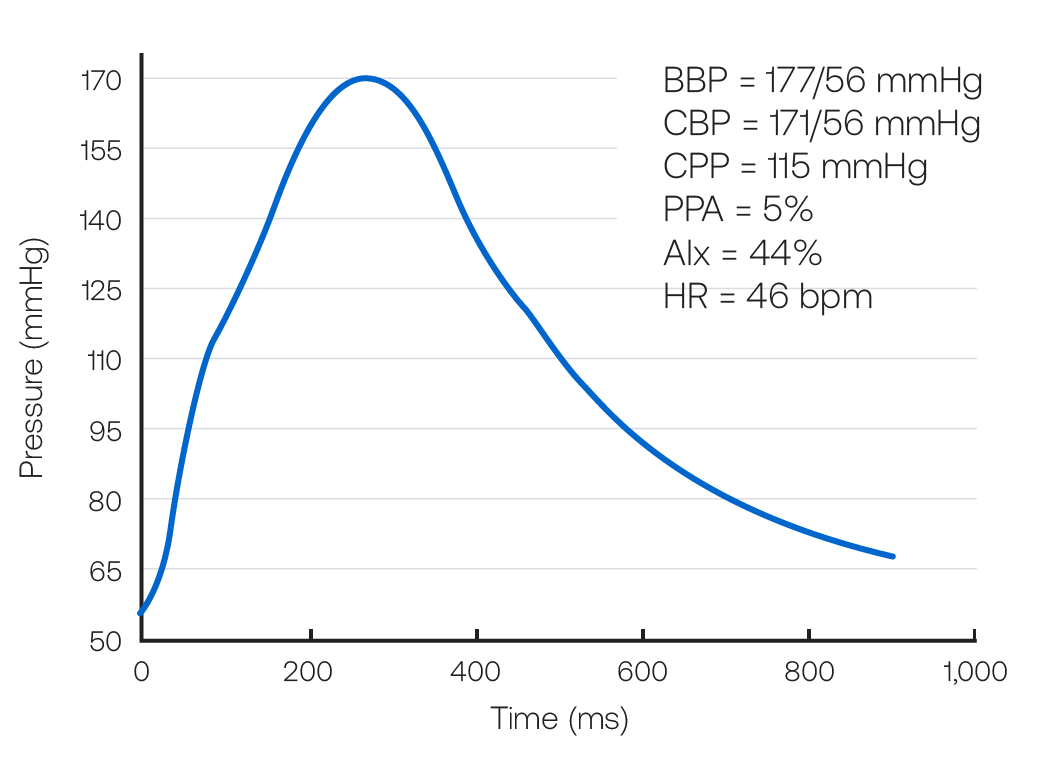
BBP indicates brachial blood pressure systolic/diastolic; CBP, central blood pressure systolic/diastolic; CPP, central pulse pressure; AIx, augmentation index; HR, heart rate; bpm, beats per minute.
Intervention
Acknowledging that this female patient is already taking several medications and has low diastolic blood pressure, there is concern about poor central pulse pressure amplification and a high brachial systolic pressure. Therefore, amlodipine 5mg daily is added, with the intention to lower brachial and central pressures but not heart rate.
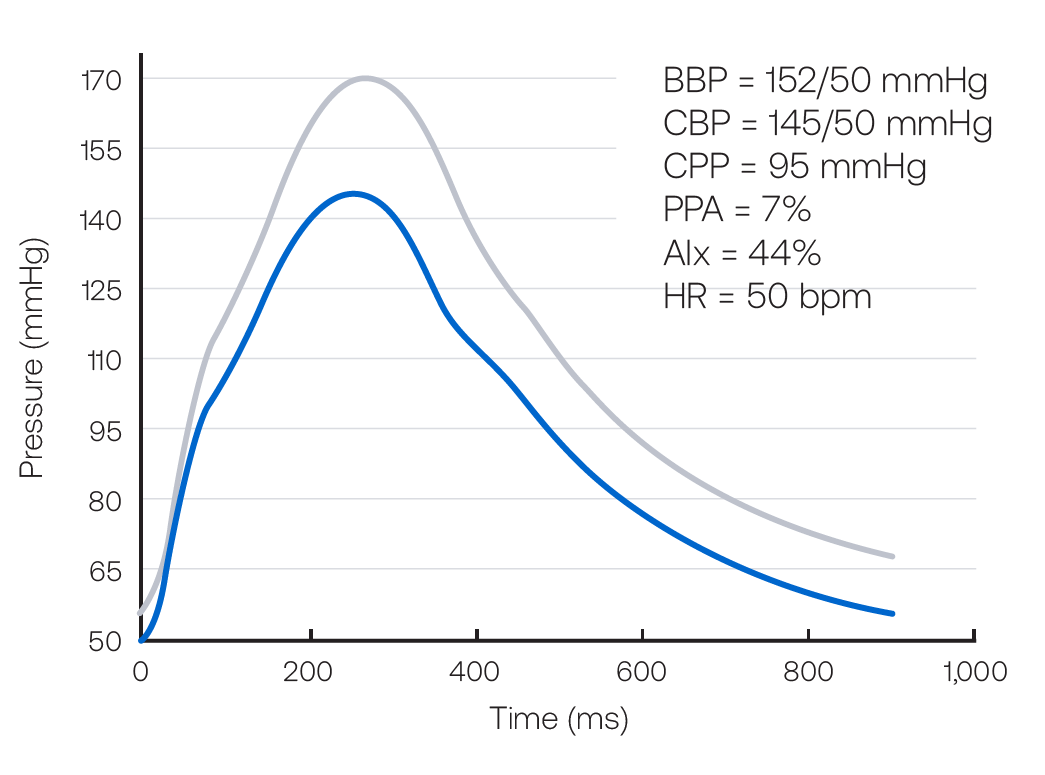
Follow Up Digital Vascular Biomarker Assessment
| Brachial Blood Pressure | 152/50 mmHg |
| Central Systolic Pressure | 145 mmHg |
| Central Pulse Pressure | 95 mmHg |
| Augmentation Index | 44% |
| Heart Rate | 50 bpm |
Follow up Assessment Interpretation
This female patient’s central pressure profile shows virtually no change in pulse pressure amplification, which was 5% and is now 7%. The central systolic pressure of 145 mmHg remains higher than the desired value of 124 mmHg. The AIx remains at about 44%. At this time, the physician decides that 50 mmHg of diastolic pressure is the limit she felt comfortable accepting and no further changes are made. In this female patient scenario, the addition of amlodipine produces an expected disproportionate decline in brachial systolic (25 mmHg) compared with brachial diastolic (6 mmHg) blood pressure. Changes in the central pressure profile provides assurance that the central pressure declines in parallel with brachial pressure. However, the central systolic pressure remains above desirable levels. The addition of vasoactive agents that selectively reduce central pressures without profoundly reducing mean arterial pressure or diastolic pressure (such as organic nitrates) may have desirable hemodynamic consequences on central hemodynamics in this context. However, no clinical guidance exists regarding the use of such agents in this setting. This should be the focus of future research.
*Townsend RR et al. Journal of Clinical Hypertension. 2015; 17:7, 503–513.
http://bit.ly/2gc5mdD
Figure 16. Central Pressure Waveform
Other Case Studies
